Spinal Stenosis
What is Spinal Stenosis?
A clue to answering this question is found in the meaning of each word. Spinal refers to the spine. Stenosis is a medical term used to describe a condition where a normal-size opening has become narrow. Spinal stenosis may affect the cervical (neck), thoracic (chest), or lumbar (low back) spine. The most common area affected is the lumbar spine followed by the cervical spine.
Are there particular spinal structures that are affected?
Yes. To help you to visualize what happens in spinal stenosis, we will consider a water pipe. Over time rust and debris builds up on the walls of the pipe thereby narrowing the passageway that normally allows water to freely flow. In the spine, the passageways are the spinal canal and the neuroforamen. The spinal canal is a hollow vertical hole that contains the spinal cord. The neuroforamen are the passageways that are naturally created between the vertebrae through which spinal nerve roots exit the spinal canal. See Figure 1.
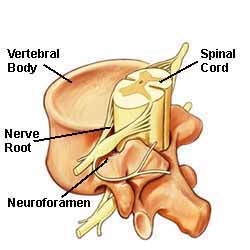
Figure 1.
The spine's bony structures encase and protect the spinal cord. Small nerve roots shoot off from the spinal cord and exit the spinal canal through passageways called neuroforamen.
Figure 2 is an artist's illustration of lumbar spinal stenosis. Notice the narrowed areas in the spinal canal (reddish-colored areas). As the canal space narrows, the spinal cord and nearby nerve roots are squeezed causing different types of symptoms. The medical term is nerve compression.
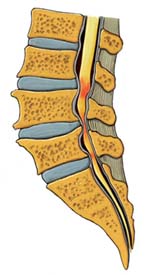
Figure 2. Lumbar spinal stenosis.
What causes Spinal Stenosis?
Some people are born with this narrowing or have a genetic tendency to develop spinal stenosis. For most people though the condition is found in patients over the age of 50. Usually spinal stenosis develops gradually as a result of aging and everyday wear the tear.
As the body ages, microscopic changes occur at the cellular level. The ligaments in the spine may thicken and harden, joints enlarge, and bone spurs (called osteophytes) form. A bulging or herniated disc is common. Most rare is a spinal tumor or spondylolisthesis; this condition develops when one vertebra slips forward onto another.
Any of these conditions can cause spinal stenosis by reducing the size of the space where the spinal cord and/or nerve roots are located. The result is nerve compression and a variety of symptoms.
What symptoms are associated with Spinal Stenosis?
First, the actual narrowing of the spinal canal or neuroforamen does not cause symptoms. Symptoms develop when the spinal cord or nerve roots are compressed; squeezed or trapped. Compression causes inflammation and inflammation can cause pain, weakness, and numbness. Symptoms vary depending on the location of the spinal stenosis. For example, the symptoms of cervical spinal stenosis primarily affect the upper body and lumbar spinal stenosis the lower body.
Cervical Spinal Stenosis
• Pain, burning or tingling sensations, feelings of pins and needles, weakness or numbness in the shoulders, arms, hands.
• Clumsy hand movement.
• Balance disturbance.
• Gait (the way a person walks) may be affected.
Lumbar Spinal Stenosis
• Pain, sciatica, tingling sensations, feelings of pins and needles, weakness or numbness in the buttocks, legs, calves.
• Symptoms may increase when walking and decrease when sitting, bending forward, or lying down.
• Rare: Bladder or bowel problems, paraplegia.
How is Spinal Stenosis diagnosed?
Similar to other medical disorders, the diagnostic process includes a complete patient history, and physical and neurological examination. You will be asked to describe your symptoms, when the condition started, activities that aggravate or alleviate symptoms, and the result of previous medications taken and therapies tried to treat the disorder.
During the physical and neurological examination the doctor will feel your spine and test your reflexes. Further, he will test your balance while watching you walk normally, on tip toes and heels. To determine how much motion you have in your spine, you may be asked to bend forward, backward, and side to side. These and other movement and reflex tests help to rule out loss of extremity reflexes, muscle weakness, and loss of feeling. The extremities are your arms and legs.
Can the doctor tell it is Spinal Stenosis just from an examination?
Depending on doctor's findings, other tests may be needed to confirm the diagnosis. These tests include:
X-Ray: An x-ray is the most common test performed and shows the structure of the spinal bones (vertebrae) and can detect bone spurs.
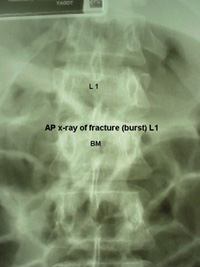
Sample X-Ray detects a spinal fracture.
MRI (Magnetic Resonance Imaging): MRI provides a highly detailed, three-dimensional image of the spine. The spinal cord, nerve roots, and spaces are clearly defined.

Sample MRI detects a spinal fracture.
CAT Scan (Computerized Axial Tomography): A CAT Scan renders images of bone better than nerves and is often used to show the shape and size of the spinal canal.
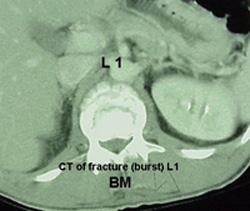
Sample CAT Scan detects a spinal fracture.
Myelogram: Using x-ray and a special liquid dye that is injected into the patient intravenously, a myelogram helps to define where there is pressure on the spinal cord or nerve roots from a herniated disc, bone spurs, or a tumor (rare).
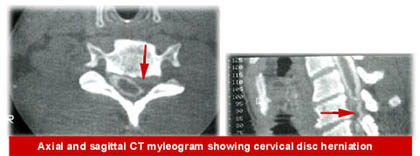
Sample Myelogram detects a cervical herniated disc.
Bone Scan: This safe test uses a radioactive material that is injected into the patient. The material attaches itself to bone and helps to detect fractures, tumors, infections, and osteoarthritis. The doctor usually relies on other tests in conjunction with a bone scan.
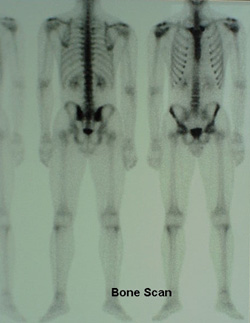
Sample Bone Scan.
Can Spinal Stenosis be treated without surgery?
Yes - in fact, less than 5% of patients with a spinal disorder ever require spine surgery!
What types of non-surgical treatments are available?
There are several non-surgical options your doctor may recommend to treat your spinal stenosis. Often, treatment combines more than one type of therapy. For example, medication may be combined with physical therapy. Let's review a few of the non-surgical therapies one by one.
Medication: There is a wide variety of medications available to relieve inflammation, pain, and muscle spasm. Although some drugs are available over-the-counter (OTC), it is wise not to combine these with prescription drugs your doctor provides unless it is under his direction. Just like prescription medications, OTC drugs can cause serious side effects.
Injections: The most common type of injection used to help alleviate the symptoms of spinal stenosis is an epidural injection. This type of injection places medication (usually a steroid) into the space that surrounds specific nerve roots (the epidural space). The medication helps to reduce inflammation and acute pain that radiates into the arms or legs. Usually a course of three injections are given over a period of several weeks.
Physical Therapy (PT): PT usually combines inactive therapy and therapeutic exercise. Inactive therapy includes heat or ice packs, ultrasound, electrical stimulation, and massage. These treatments help to ready the patient for active therapy by relaxing tight muscles and easing pain or discomfort. Therapeutic exercise includes stretching and prescribed exercises to help stabilize the spine, build strength and endurance, and increase flexibility.
What happens if I'm one of the 5% that needs surgery?
Surgery, any kind of surgery is a serious decision. Your doctor will take sufficient time to thoroughly explain your surgical options with you. You might consider bringing a family member or friend along for an added set of 'ears'.
A few patients do require spine surgery to treat the symptoms caused by spinal stenosis. The goal of surgery is to relieve the pressure on the spinal cord and/or nerve roots. This is accomplished by enlarging the spinal canal and/or neuroforamen. The type of surgical procedure performed depends on the type, location, and cause of the spinal stenosis.
What is the name of the surgical procedure?
There are several different surgical procedures used to treat spinal stenosis. Listed below are the names and a brief description of each procedure. Once again, your doctor will explain which procedure or procedures will be performed during your operation.
Laminotomy: The lamina is a small, thin bony spinal structure located at the back of the spine (posterior) that covers access to the spinal canal and spinal cord. A small portion of the lamina may be removed to relieve pressure on the nerve roots.
Decompressive Laminectomy: This is the most common surgical procedure performed in the lumbar spine. The lamina is removed to decompress or relieve pressure on the nerves.
Foraminotomy: During this procedure, the neuroforamen are enlarged. Sometimes this procedure is combined with a laminotomy.
Medial Facetectomy: One of the causes of spinal stenosis is one or more enlarged joints. The spinal joints are named facet joints. During this procedure part of the facet joint is removed to increase space.
Anterior Cervical Discectomy and Fusion (ACDF): This procedure removes a diseased disc (discectomy) through the front (anterior) of the neck (cervical). After the disc is removed, the spine must be stabilized. This is accomplished using a cervical plate and screws (instrumentation) and fusion (bone graft). Fusion is similar to glue that hardens over time to create a solid construct, which stabilizes the spine.
Lumbar Discectomy and Fusion: This is similar to ACDF, except entry into the spine may be gained through the front (anterior), back (posterior), or side (transforaminal).
Cervical Corpectomy: During this procedure, part of the vertebra and adjacent disc are removed to decompress the cervical spinal cord and nerve roots. Instrumentation and fusion are performed to permanently stabilize the spine.
Will the surgical procedure take away my pain?
This is a good question. Your doctor will provide you with statistics that help to predict your surgical outcome. These statistics are important and will help you to determine if surgery is the best choice.
If your nerves were badly damaged before surgery, you may experience some pain or numbness afterward. Sometimes there is no improvement at all. Unfortunately, as you age your spine will continue to change or degenerate. Sometimes symptoms reappear several years after surgery.
How long will it take me to recover and get back to my life?
This depends on the type of surgical procedure and your condition before surgery. Some spine procedures can be performed on an outpatient basis that allows you to go home the same day. A more comprehensive procedure, such as one involving fusion requires hospitalization.
At an appropriate time after surgery, your doctor will prescribe a course of physical therapy. This gives patients a good step forward in their recovery and return to everyday activities.
All illustrations are courtesy of www.spineuniverse.com
